The Liquid-Based Cytology (LBC) test and the Conventional Pap Smear are both critical diagnostic tools used for screening cervical cancer and detecting abnormal cellular changes. While they share similar objectives, their methods of sample collection, processing, and diagnostic accuracy differ significantly. This comparison delves into the strengths and weaknesses of each technique, highlighting factors like sample preservation, diagnostic sensitivity, and accessibility, helping healthcare providers make informed decisions when choosing between the two.
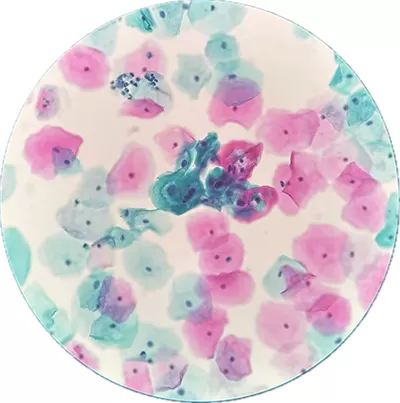
The LBC test (Liquid-Based Cytology test) is an advanced laboratory technique used for microscopic examination of cells. Unlike conventional methods, it involves suspending collected cells in a liquid medium, which helps remove debris and preserve cellular integrity. This approach enhances sample quality, reduces contamination, and improves diagnostic accuracy.
By utilizing automated processing, the LBC test ensures a more uniform and concentrated cell sample, making microscopic analysis more efficient and reliable. It minimizes the risk of inadequate specimens, leading to more consistent and reproducible results. Additionally, the liquid-based preparation allows for ancillary testing, optimizing laboratory workflows and efficiency.
With its improved sensitivity and specificity, the LBC test represents a significant advancement in cytological examination, supporting more accurate and dependable cellular analysis. Its widespread adoption has contributed to the evolution of modern diagnostic techniques, offering enhanced precision in detecting cellular abnormalities.
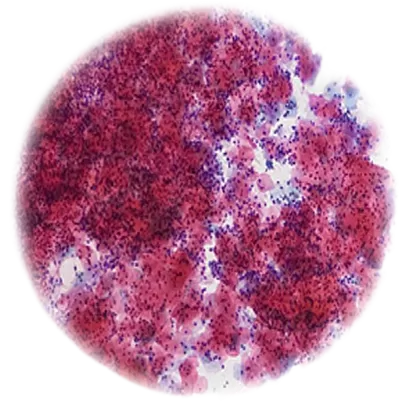
A Pap smear test, also known as a Pap test, is a laboratory procedure used to examine cells collected from the cervix. It is designed to detect cellular changes, abnormalities, and potential health risks at an early stage.
During the test, a small sample of cervical cells is collected using a brush or spatula and then spread onto a glass slide or suspended in a liquid medium for microscopic analysis. This process helps identify irregular cell growth, ensuring timely medical evaluation.
The Pap smear is a routine and essential test known for its reliability in detecting cellular changes. It is a simple, quick, and minimally invasive procedure, typically performed during routine health check-ups. By providing valuable insights into cellular health, the Pap smear test plays a critical role in diagnostic cytology, contributing to early detection and further medical assessments when necessary.
1. Sample Collection & Preparation
Liquid-Based Cytology (LBC): Cells are collected from the cervix using a brush or spatula and placed in a liquid solution. This method ensures cells are suspended and prevents them from drying out. The liquid medium helps eliminate blood, mucus, and other contaminants, ensuring that only the highest-quality cells are analyzed, which improves overall sample quality. The sample is then processed to produce a uniform, even layer of cells for examination.
In Conventional Pap Smear method, cells are scraped directly from the cervix and spread onto a glass slide. The sample is then air-dried, which can lead to cell distortion or loss. Blood, mucus, or other debris may obscure the sample, making it harder for pathologists to assess. This process can result in less consistent cell distribution, increasing the risk of inaccurate results or false negatives.
2. Diagnostic Accuracy & Sensitivity
Using Liquid-Based Cytology Equipement is more accurate due to its improved sample preparation. The liquid medium ensures that only the best cells are preserved and analyzed, which enhances the detection of abnormal cells and reduces the occurrence of false negatives. The method's higher sensitivity and precision also make it better suited for identifying early-stage abnormalities and infections, such as HPV, that may lead to cervical cancer.
The accuracy of conventional Pap smears can be compromised due to improper sample collection, uneven slide preparation, and the possibility of cell overlap or drying. This can increase the likelihood of false negatives, where abnormal cells are missed. Additionally, the manual process may lead to human error in interpreting results, further reducing diagnostic accuracy compared to LBC.
3. Sample Preservation & Contamination
One of the key advantages of LBC is its ability to preserve cell integrity during transportation and processing. The liquid medium helps maintain the cells in their natural state, reducing the risk of contamination by blood, mucus, or other foreign substances. This preservation ensures that pathologists receive a clearer, more accurate sample for analysis, which enhances the overall diagnostic reliability of the test.
Sample preservation in conventional Pap smears is more prone to issues. The cells are spread directly onto the slide and can dry out quickly, leading to potential distortions. Furthermore, contamination from blood, mucus, or even bacteria can obscure the cells, making it difficult to properly assess for abnormalities. The lack of a preservation medium reduces the quality of the sample over time.
4. Efficiency in Processing & Testing
Liquid-Based Cytology Machine streamlines the laboratory process with greater automation. The liquid suspension allows for easier handling and processing, reducing the time spent on manual slide preparation. This method is more efficient as it allows the same sample to be used for additional tests, such as HPV screening or other molecular analyses, without needing to collect a separate sample. This results in quicker turnaround times and more comprehensive testing.
The conventional method requires manual slide preparation, which can be time-consuming and labor-intensive. Each sample needs to be handled individually, and the risk of human error in the preparation process is higher. If additional testing is required (e.g., for HPV), a separate sample must be collected, adding time and complexity to the overall diagnostic process. This inefficiency may delay results and increase the potential for inaccuracies.
5. Cost & Accessibility
While LBC is generally considered more accurate and efficient, it tends to be more expensive due to the specialized equipment, processing technology, and reagents involved. Additionally, the need for advanced laboratory infrastructure can make it less accessible in resource-limited settings. Despite the higher cost, the improved diagnostic accuracy justifies the investment, especially in developed healthcare systems where precision is a priority for early disease detection.
Conventional Pap smears are typically less expensive and more widely available, especially in regions with limited healthcare resources. They do not require advanced technology or equipment, making them a cost-effective option for routine screenings. However, the lower cost comes at the expense of diagnostic sensitivity and accuracy, which can lead to higher follow-up rates for patients. This may offset the initial savings in healthcare costs by necessitating further testing.
6. Turnaround Time for Results
LBC typically offers a quicker turnaround time for results due to the streamlined processing and automation involved in the preparation and analysis. The uniformity of the sample and the use of advanced equipment allow laboratories to process more samples efficiently, which reduces delays. In some cases, the same sample can be used for multiple tests, speeding up the diagnostic process and providing comprehensive results faster.
The turnaround time for conventional Pap smears can be longer due to the manual preparation process and the need for rework if the sample is inadequate. Slides may need to be retaken if the initial preparation is unsatisfactory. The reliance on human intervention during sample collection and slide preparation increases the likelihood of errors, potentially delaying results as labs may need to repeat tests to ensure accuracy.
7. Human Error & Interpreting Results
LBC reduces the potential for human error by automating many parts of the preparation process. With fewer variables in the sample collection and processing stages, pathologists receive more consistent, high-quality slides to analyze. Additionally, the uniform distribution of cells allows for more accurate and consistent interpretations, leading to fewer misinterpretations or missed abnormalities during the diagnostic process.
Because conventional Pap smears involve more manual steps—such as spreading the sample on a slide and drying—it increases the likelihood of human error. For example, a poorly prepared slide may result in incorrect interpretations or lead to missed abnormalities. Pathologists may also find it more difficult to distinguish certain types of abnormalities if the cells are unevenly distributed or obscured by contaminants, ultimately impacting diagnosis accuracy.
| Feature | Liquid-Based Cytology (LBC) | Conventional Pap Smear |
| Sample Collection | Cells placed in liquid to prevent drying and contamination. | Cells spread on a slide, can dry out and be uneven. |
| Accuracy | More accurate, fewer false negatives. | Less accurate, higher chance of missed abnormalities. |
| Sample Preservation | Liquid keeps cells intact and clean. | Cells can dry out and get contaminated. |
| Processing | Automated, faster, and allows extra tests (e.g., HPV). | Manual, slower, extra tests need a new sample. |
| Cost | More expensive, needs special equipment. | Cheaper, widely available. |
| Turnaround Time | Faster due to automation. | Slower due to manual steps. |
| Human Error | Less error, consistent results. | More error due to manual handling. |
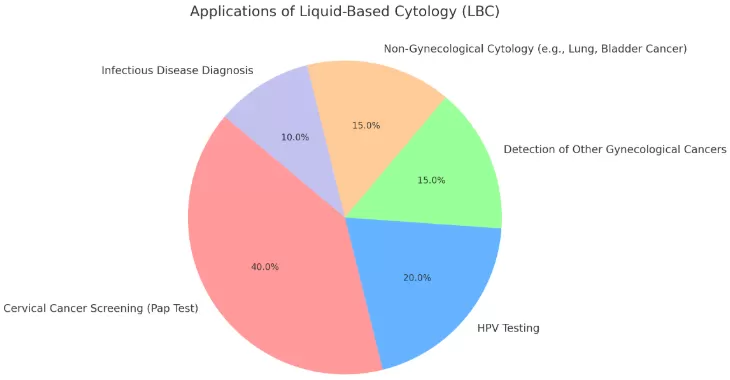
Liquid-Based Cytology (LBC) is widely used in cervical cancer screening to detect abnormal or precancerous cells in the cervix. It improves the accuracy of Pap tests by suspending cells in a liquid medium, reducing contamination and ensuring better sample quality. Additionally, LBC is essential for HPV testing, helping identify high-risk strains of the virus that may lead to cervical cancer, making it a crucial tool for early detection and prevention.
Beyond cervical screening, LBC is used in diagnosing various gynecological and non-gynecological conditions. It helps detect cancerous or abnormal cells in body fluids, such as urine cytology for bladder cancer screening and respiratory cytology for lung cancer detection. Additionally, LBC is employed in lung infection diagnosis, where it enhances the identification of lung infections and malignancies by providing clearer, more reliable samples for microscopic examination, improving the overall accuracy of test results.
LBC is also valuable in identifying infectious diseases and analyzing fine-needle aspiration (FNA) samples. Its ability to preserve cells effectively makes it useful for diagnosing bacterial, viral, and fungal infections in different tissues. In addition, it plays a key role in evaluating FNA samples from breast lumps and thyroid nodules, aiding in early cancer detection. The improved sample quality and reduced contamination risk make LBC a preferred method in modern cytological testing.
Choosing between Liquid-Based Cytology (LBC) and a Conventional Pap Smear depends on several factors, including diagnostic accuracy, healthcare infrastructure, and cost considerations. LBC is preferred in settings where high sensitivity, precise results, and the ability to conduct additional tests, such as HPV screening, are crucial. It is more efficient and accurate, reducing the chances of false negatives. On the other hand, conventional Pap smears may be chosen in areas with limited resources due to their lower cost and widespread availability. The decision often balances medical needs, budget constraints, and access to advanced laboratory facilities.